Fertility Inositol FAQs
About Our Research
We have built a research bot based on the Evidence Based Guidelines and our own peer reviewed journal article research. Please ask it anything and let us know if it is helpful.
Hi👋 I am Jai, Inositol.au's chatbot assistant! I am trained on the sites content and Evidence Based Guidelines. Here are some things you can ask me:
• What do the PCOS guidelines say about diet and exercise?
• How can inositol help with PCOS symptoms?
• What are the guideline recommendations for fertility treatment?
• Where is my order? (Must be logged in)
Just ask anything. I am still learning about my new job, but I'll give you the best answer I can.
Medical Disclaimer: Please note we are not doctors and are not qualified to give medical advice. The information on this site is general in nature and does not take into account your specific health circumstances. Nothing on this site should be a substitute for professional health or medical advice.

FAQs
The issue of PCOS patients over-converting MI to DCI, is identified as a key mechanism underlying the “D-chiro-inositol (DCI) ovarian paradox.”
Here’s what the research reveals:
The Over-Conversion Problem
The report describes how PCOS patients with hyperinsulinemia commonly present “increased levels MI to DCI epimerisation, leading to an MI deficiency in the ovaries, resulting in impaired folliculogenesis, anovulation, and decreased oocyte quality” . This over-conversion is mediated by insulin-stimulated epimerase activity, where “insulin can stimulate enzymatic activity in the ovaries, leading to an increase in the DCI/MYO conversion rate” .
Tissue-Specific Requirements
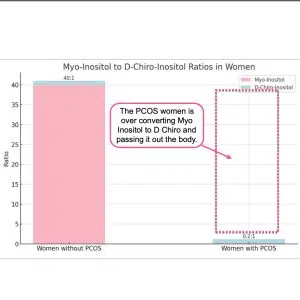
The research emphasises that different tissues have vastly different inositol requirements. The physiological ovarian MI/DCI ratio is 100:1, which is “much higher” than the serum ratio of 40:1, “with a greater need for MI due to its role in FSH signaling” . This suggests that ovaries are particularly vulnerable to MI deficiency when conversion rates increase.
The Paradox Mechanism
Multiple studies describe what’s termed the “D-chiro-Ins ovarian paradox” . In PCOS ovaries, “increased epimerase activity leads to local Myo-Ins deficiency” which “may adversely affect glucose uptake and metabolism of both oocytes and follicular cells” . This creates a situation where the ovary becomes depleted of the specific inositol form it needs most.
Clinical Evidence of Over-Conversion Effects
The research provides clinical evidence that this over-conversion is problematic. Isabella et al. demonstrated that “increasing DCI dosage progressively worsens oocyte quality and ovarian response” in non-insulin-resistant PCOS patients . This suggests that adding more DCI (the end product of conversion) when conversion is already excessive can further harm ovarian function.
Functional Consequences
The over-conversion has specific functional consequences because MI and DCI serve different roles: “MI increases glucose cellular uptake and D-chiro-Ins is involved in glycogen synthesis” . Since ovaries require glucose uptake for proper function rather than glycogen storage, the shift toward DCI production impairs ovarian metabolism.
Treatment Implications
This over-conversion research suggests that PCOS treatment should focus on restoring MI availability rather than providing more DCI. The research indicates that “myo-inositol treatment rather than D-chiro-inositol is able to improve oocyte and embryo quality during ovarian stimulation protocols” in euglycemic PCOS patients , supporting the idea that correcting MI deficiency is more important than adding DCI. The research comprehensively addresses this over-conversion issue as a central mechanism explaining why standard 40:1 ratios may be inappropriate for many PCOS patients, particularly those undergoing fertility treatments.
Based on the research report, here are the key citations specifically relating to the over-conversion paradox:
Primary References for the Over-Conversion Paradox:
V. Unfer et al., 2016 – This is the most comprehensive source, describing:
- The “D-chiro-Ins ovarian paradox” concept
- How increased epimerase activity in PCOS ovaries leads to local MI deficiency
- Tissue-specific ratios (100:1 in ovary vs 40:1 in serum)
- How reduced intraovarian MI affects glucose uptake and oocyte metabolism
O. Pustotina et al., 2024 – Provides detailed mechanistic explanation:
- How hyperinsulinemic patients present “increased levels MI to DCI epimerization”
- The physiological ovarian ratio being 100:1 vs serum 40:1
- Warning that “high doses and prolonged DCI use can block aromatase expression and lead to hyperandrogenism”
R. Isabella et al., 2012 – Describes the clinical paradox:
- Proposes the “D-chiro-inositol paradox in the ovary of PCOS patients”
- Explains how PCOS patients with hyperinsulinemia have “enhanced MI to DCI epimerization rate in the ovary”
- Shows that “MI depletion could eventually be responsible for the poor oocyte quality”
N. Mendoza et al., 2017 – Supports the conversion mechanism:
- Documents how “insulin can stimulate enzymatic activity in the ovaries, leading to an increase in the DCI/MYO conversion rate”
- Notes “contradictory results on DCI effectiveness in ovarian tissue”
Supporting Evidence:
V. Unfer et al., 2011 – Provides clinical evidence of the paradox effects in euglycemic PCOS patients undergoing ICSI
M. Nordio et al., 2019 – Shows that “too much DCI causes a loss of beneficial effects at the reproductive level”
We recommend a dose of 4g per day taken as 2g in the morning with breakfast and 2g taken in the evening with dinner.
The inositol problem in PCOS is that the body over converts Myo Inositol (MI) into D Chiro Inositol. (DCI) Adding more DCI isn’t the answer.
In PCOS patients with hyperinsulinemia, increased epimerase activity leads to excessive conversion of MI to DCI in the ovary, resulting in MI depletion and DCI overproduction (Nestler & Unfer, 2015; Unfer et al., 2014).
This imbalance may impair FSH signaling and oocyte quality (Nestler & Unfer, 2015). Studies have shown that the MI:DCI ratio in follicular fluid drops from 100:1 in healthy women to 0.2:1 in PCOS patients (Unfer et al., 2014).
The altered MI:DCI ratio may contribute to pathological steroidogenesis in PCOS, with DCI promoting androgen synthesis and reducing estradiol production (Unfer et al., 2020).
Restoring the appropriate MI:DCI ratio has shown efficacy in PCOS treatment, and MI supplementation may improve oocyte and sperm quality in assisted reproduction (Facchinetti et al., 2016).
In addition D-Chiro has negative long term effects.
Please read:
Nordio, M.; Bezerra Espinola, M.S.; Bilotta, G.; Capoccia, E.; Montanino Oliva, M. Long-Lasting Therapies with High Doses of D-chiro-inositol: The Downside. J.Clin. Med. 2023, 12, 390. https://doi.org/10.3390/jcm12010390
R. GAMBIOLI, G. FORTE, C. ARAGONA, A. BEVILACQUA, M. BIZZARRI, V. UNFER. The use of D-chiro-Inositol in clinical practice European Review for Medical and Pharmacological Sciences 2021; 25: 438-446
The 40:1 ratio contains 2.5-fold more d-chiro-inositol than the physiological ovarian requirement (100:1), creating relative DCI excess that impairs oocyte quality, increases FSH requirements, and can block aromatase activity—making it suboptimal for fertility outcomes particularly in assisted reproduction, despite effectiveness for restoring ovulation in insulin-resistant anovulatory patients.
The available evidence suggests the 40:1 myo-inositol to d-chiro-inositol (MI/DCI) ratio demonstrates context-dependent efficacy rather than being universally “wrong” for PCOS and fertility. The ratio appears effective for restoring ovulation in anovulatory, insulin-resistant patients seeking natural conception, but multiple lines of evidence indicate it may be suboptimal for oocyte quality during assisted reproduction. Head-to-head comparisons consistently favor MI over DCI for fertility outcomes in ART contexts, with Isabella et al. demonstrating dose-dependent deterioration in oocyte quality, embryo quality, and FSH requirements as DCI doses increase from 300 to 2400 mg. Mechanistically, the physiological ovarian MI/DCI ratio is 100:1—approximately 2.5-fold higher than the 40:1 ratio used in supplements—suggesting the 40:1 formulation contains excessive DCI relative to ovarian tissue requirements. The “D-chiro-inositol ovarian paradox” explains that increased epimerase activity in PCOS ovaries already creates local MI deficiency, which exogenous DCI at 40:1 may exacerbate rather than correct. Furthermore, high DCI doses can block aromatase expression and paradoxically cause hyperandrogenism, potentially impairing fertility despite systemic metabolic benefits. However, the evidence does not conclusively prove 40:1 is wrong for all PCOS patients: it may represent an acceptable compromise for anovulation when systemic insulin sensitization is needed, but appears excessive for euglycemic patients or those prioritizing oocyte quality in assisted reproduction, where ratios approaching the physiological 100:1 may be preferable.
Read the full report here: Why 40:1 myo-inositol to d-chiro Inositol is wrong for PCOS and Fertility
References
(2012). CONCERN: Does ovary need D-chiro-inositol?. Journal of Ovarian Research
Myo-inositol begins restoring ovulation within 3-5 weeks but achieves optimal pregnancy rates after 3-6 months of sustained treatment.
Myo-inositol demonstrates a hierarchical timeline of fertility effects, with the earliest measurable responses occurring within 1 week. Estradiol concentrations increased within the first week of treatment, representing the initial hormonal response. Functional ovulatory restoration occurred more gradually, with time to first ovulation at 24.5 days (95% CI: 18-31 days) compared to 40.5 days for placebo, and 88% of PCOS women experiencing their first spontaneous menstrual cycle after a mean of 34.6±5.5 days. Clinical pregnancies required sustained treatment, with large observational cohorts documenting 70% ovulation restoration and 15.1% pregnancy rates by 10.2 weeks, while extended 6-month protocols achieved 40% pregnancy rates. Significant hormonal changes, including testosterone reduction and progesterone elevation, were consistently documented after 12 weeks.
The optimal treatment duration depends on therapeutic context. For women seeking spontaneous conception, treatment should be sustained for 3-6 months to maximize pregnancy outcomes, while ovulatory effects become apparent within 4-5 weeks. For IVF protocols, 1-2 months of pre-treatment improved oocyte quality and fertilization rates. However, most studies were not designed with timing as a primary endpoint, and only one trial provided confidence intervals for time-to-event outcomes. The evidence suggests a dose-response relationship between treatment duration and pregnancy rates, though individual response varies based on baseline characteristics such as BMI
Full research report here: How long does it take for myo-inositol to work for fertility.
References
E. Papaleo, V. Unfer, J. Baillargeon, L. De Santis, F. Fusi, and 5 more
Still have questions? Check out our Inositol General FAQs and our PCOS Inositol FAQs
Shop Inositol
$ 33.00 – $ 198.00Price range: $ 33.00 through $ 198.00
Learn More

Berberine vs. D-Chiro-Inositol: Which Is Better for Insulin Resistance in PCOS?
1. Introduction If you’re trying to manage PCOS, you’ve likely come across supplements like inositol or berberine. But not all insulin-sensitising supplements are created equal

What Is Inositol Used for in the Body?
Inositol is a substance that can have many beneficial effects on your body. But how exactly does it work, what is Inositol used for and

The Best Pre Fertility Checklist
Last Revised 09/05/2022 When considering fertility, it’s a good idea to develop a pre fertility checklist. This checklist will help you and your partner plan

Getting Pregnant With Insulin Resistance: Here’s 5 Things You Need To Know
Photo by Cody Black on Unsplash Having a child is a life-changing experience, but when you are getting pregnant with insulin resistance with complications or are at high-risk,

Inositol Powder for Fertility
If you’ve ever experienced trouble with fertility, then you know that it can be the worst feeling in the world. Not only are you eager

What is Vitamin B8?
Every day we consume numerous sugars, vitamins, and minerals that are vital to the healthy functioning of our body. We are told to consume a