With a quarter of the population believed to have some form of insulin resistance, it is a significant health concern that people need to be aware of.
Insulin resistance is a condition where cells in fat, muscles, and the liver are unable to properly process insulin. Ordinarily, the insulin produced by the pancreas is used by the cells to help them take up glucose from the blood to use for energy.
For people with insulin resistance, the glucose does not get used and insulin continues to be produced. Eventually, this causes increased blood glucose levels and leads to conditions like type 2 diabetes and the cluster of cardiovascular disease symptoms known as metabolic syndrome.
But for many, questions remain about the cause of insulin resistance. Is insulin resistance genetic? Or is it the result of lifestyle choices and/or other medical conditions?
In this blog, we go over whether or not insulin resistance is genetic and what you can to improve insulin resistance in the body.
Is Insulin Resistance Genetic?
Insulin normally helps regulate blood sugar levels, but unfortunately that function can sometimes fail.
Insulin resistance is the body’s inability to properly take in insulin. And unfortunately, severe insulin resistance can lead to severe health problems:
- High blood sugar
- Severe metabolic health
- Prediabetes
- Type 2 diabetes
- Metabolic syndrome, which refers to a cluster of cardiovascular risk factors including high blood pressure, which can lead to diabetes and stroke.
- Insulin resistance can also turn into a severe version, known as type A insulin resistance syndrome.
For the many health problems that insulin resistance is associated with, many people wonder is insulin resistance genetic and, in turn, if it can be avoided.
Unfortunately, the answer as to whether or not insulin resistance is genetic is not as simple as a straightforward “yes” or “no.”
Like many things in life, it is complicated.
Genetic Factors and Insulin Resistance
Recent research has identified some common and rare genetic variations associated with insulin resistance, including the function of the insulin receptor and insulin secretion. Many of the genetic variant types identified as being associated with insulin resistance are directly related to glucose metabolism.
A Harvard study has hinted that the human gene variant NAT2 might play a role in insulin resistance. And, by proving that this or another gene is a primary player in causing insulin resistance, then researchers could essentially stop insulin resistance before it gets worse and causes type 2 diabetes and other health problems.
Unfortunately, further study is required to identify the ways in which these, and other, gene expression variants contribute to the development of insulin resistance.
According to the American Diabetes Association, other factors that contribute to an increased risk of developing insulin resistance syndrome include:
- A family history of diabetes
- Race. Black, Hispanic, and Indigenous populations are more at risk
- A family history of PCOS
- Lifestyle
PCOS and Insulin Resistance
PCOS, or poly-cystic ovarian syndrome (PCOS), is a major potential risk factor for developing insulin resistance.
Insulin resistance is one of the primary imbalances experienced by many women with PCOS. Women diagnosed with this condition are often less effective at using insulin and usually have a high blood sugar level.
While the exact link between PCOS and insulin resistance is not entirely clear, it is clear that they are connected. It is estimated that half of women diagnosed with PCOS will develop type 2 diabetes by the time they are 40.
According to Dr. Abed-Alwahab, “Insulin is a fat-storage hormone that concentrates fat in your abdominal region. High insulin levels can tell the ovaries to make more testosterone. That’s why some women with PCOS have symptoms of excess androgens, like dark hairs on the face and belly.”
What is clear about PCOS and insulin resistance is that they exacerbate one another and by working to treat and manage one, can help treat and manage the other.
Lifestyle Factors and Insulin Resistance
Genetics is not the only thing that can play a role in developing insulin resistance. There are many lifestyle factors that come in to play as well.
Lifestyle factors that increase the risk for insulin resistance include:
- Obesity
- Stress
- Sedentary lifestyle
- Smoking
- High-carb diet
The good news is that many of these lifestyle factors may be changed or controlled, potentially improving insulin sensitivity and reversing insulin resistance.
Tips for Reversing or Reducing the Risk of Developing Insulin Resistance
While we know that making lifestyle changes is easier for some than it is for others, we know that making relatively simple changes in diet and activity level can significantly change your insulin resistance, helping to manage or even reverse the condition.
Even with a genetic connection, insulin resistance does not have to be your fate!
Here are some things you can do to naturally reduce insulin resistance:
Move Your Body
Adding a little bit of exercise and movement to your daily routine can go a long way to controlling glucose levels and improving insulin sensitivity.
Exercise helps each muscle cell, fat cell, and liver cell absorb blood glucose better. Our muscles use glucose for energy during physical activity and when the activity is done, they need to replenish those energy stores and they do so by removing glucose from the blood.
While vigorous exercise is “better,” in that it uses more energy so, in turn, more energy or glucose needs to be replaced.
But, don’t think you need to go out and immediately start some expert level, intense training regimen. Some activity is better than no activity.
The Australian Government Department of Health recommends 2.5 to 5 hours of moderate activity or 1.25 to 2.5 hours of vigorous activity or an equivalent combination of both, per week.
When you think about it, 2.5 to 5 hours of moderate activity per week is really not that much! And smaller bouts of 10 minute workouts can quickly add up over time!
Consistency is important here so seek out activities that elevate your heart rate but are not too difficult or uncomfortable for you to do. It is important to exercise at your fitness level. If you start too intensely or doing an activity that is unreasonably painful, you will likely give up and reduce the beneficial returns.
Walk, hike, cycle, swim, run. Whatever works for you.
For some workout ideas, check out these exercise plans for women with insulin resistance.
Eat Healthier
Diets high in processed foods and carbohydrates can contribute to the development of insulin resistance.
The “simplest” solution is to avoid excessive carbs and pre-packaged, processed foods. Of course, that’s not to say that this will necessarily be easy.
Start by removing these types of foods from your pantry and replace them with healthier options like fresh fruits and vegetables. Nuts and seeds, cheese, or Greek yogurt can also be a nutritious fit when looking for a snack.
This transition may be difficult for some so it is important to focus on the positives. Any change made towards a healthier diet is a positive change. Some may be able to make wholesale changes immediately, others may need to take baby steps.
If you are uncertain about the dietary changes you need to make, reach out to your physician, nutritionist, or dietitian for direction and advice.
Try a Natural Supplement
While there is no magic pill or supplement that can guarantee glucose tolerance or insulin action, there are some things you can take that will help improve the condition.
A supplement like Myo-Inositol can help improve metabolic function if you are experiencing insulin resistance due to PCOS or gestational diabetes.
Myo-Inositol is a vitamin-B complex that works to help regulate cellular response. It has been shown to be effective at improving insulin sensitivity and reducing insulin resistance.
Studies in postmenopausal women, women with gestational diabetes, and women with PCOS have all demonstrated improvements in insulin resistance after ingesting Inositol. This powerful herbal supplement can improve insulin signaling and provide significant metabolic disease control effects.
Shop Inositol Australia
While insulin resistance has no single cause: it could be related to genetics or it could be your lifestyle, it also has no single resolution.
Along with increased exercise, weight loss, and a healthier diet, supplementing with Inositol can help manage out of an control insulin level and reduce the signs of insulin resistance. Inositol Australia has a range of natural GMO-free products to support a number of conditions, including insulin resistance.
Contact us today to learn more!
-
Natural Myo Inositol for Insulin Resistance$ 34.95 – $ 209.95
-
Nature’s Sunshine Berberine – 90 Capsules$ 49.95
-
Morlife Collagen Protein Water – 400g – Tropical or Berry$ 54.95
-
Morlife Beauty Collagen Antiox – Berry Deluxe 200g$ 49.95
-
Morlife Marine Collagen + Vitamin C – Unflavoured 200g$ 39.95
-
Morlife Plantiful Protein Powder – 440g – Chocolate or Vanilla Fudge$ 44.95
-
Morlife Alkalising Greens – Berry Burst 200g$ 44.95
-
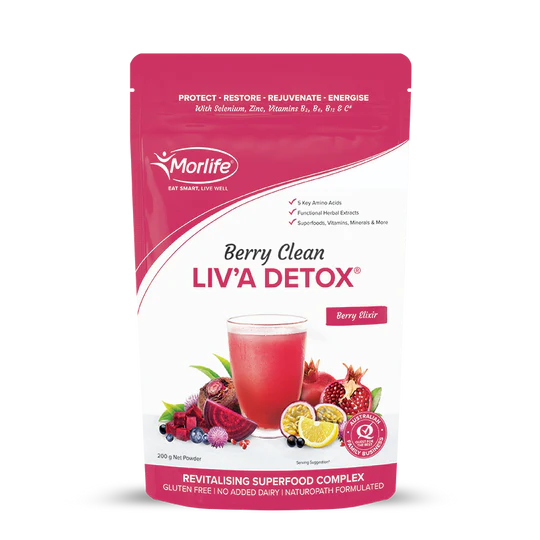
Morlife Berry Clean Liva Detox – Berry Elixir 200g$ 44.95
-
Vital Zing Water Drops$ 6.45
Sources
Better Health Channel. (2022). Metabolic syndrome. Retrieved Feb 24, 2022.
Australian Family Physician. (2022). The Metabolic Syndrome. Retrieved Feb 24, 2022.
Audrey E. Brown and Mark Walker. (2016) Genetics of Insulin Resistance and the Metabolic Syndrome. Current Cardiology Reports. 18:75. Retrieved Feb 24, 2022.
Inositol Australia (2022). PCOS and Diabetes. Retrieved Feb 24, 2022.
Cleveland Clinic (2022). Controlling Your Blood Sugar Can Improve Your PCOS and Hormone Imbalance. Retrieved Feb 24, 2022.
WebMD (2022). Insulin Resistance: Symptoms, Causes, Tests, Treatment. Retrieved Feb 24, 2022.
Inositol Australia (2022). How To Treat Insulin Resistance Naturally. Retrieved Feb 24, 2022.
Diabetes.co.uk (January 15, 2019). Insulin Sensitivity. Retrieved Feb 24, 2022.
Commonwealth of Australia (2022). Physical activity and exercise guidelines for all Australians. Department of Health. Retrieved Feb 24, 2022.
Inositol Australia (2022). 3 Best Insulin Resistance Exercise Plans for Women. Retrieved Feb 24, 2022.
Inositol Australia (2022). Inositol for PCOS | Inositol Australia | Vitamin B8 | Myo Inositol Powder. Retrieved Feb 24, 2022.
Inositol Australia (2022). Inositol for Gestational Diabetes. Retrieved Feb 24, 2022.
Healthline (2022). 5 Evidence-Based Health Benefits of Inositol. Retrieved Feb 24, 2022.
American Diabetes Association (2022). Genetics of Diabetes. Retrieved Feb 25, 2022.
Medline Plus: Genetics (2022). Type A insulin resistance syndrome. Retrieved Feb 25, 2022.Arturo Bevilacqua and Mariano Bizzarri. (2018) Inositols in Insulin Signaling and Glucose Metabolism. International Journal of Endocrinology. doi: 10.1155/2018/1968450